Want to learn more about the context for our lab’s work? Check out the sections below to learn more about the field of healthcare sustainability and what life cycle assessment means.
The Impacts of Climate Change on Health, Especially Cancer Care
Climate change impacts on human health are well-documented and projected to further increase if mitigation responses remain inadequate. Rising temperatures directly exacerbate the frequency and intensity of extreme weather events including wildfires, hurricanes, floods, and droughts. Such events threaten not only our ecological community but also the health of our population. As weather patterns change, the prevalence of vector-borne illnesses, contamination of food and water, reduction in crop yields and their nutritional value, and socio-political conflicts will continue to increase. Furthermore, diminished air quality and pollution will exacerbate and increase the prevalence of many health conditions, including respiratory disease and cancers such as lung, gastrointestinal, and skin. Climate change further magnifies health disparities, as the effects have a disproportionate impact on the most vulnerable populations (e.g., older populations, children, low-income populations, ethnic minorities, and patients with chronic conditions, including cancer) who are the least equipped to deal with these effects.
Impact of climate change across the cancer care continuum:

Reference: https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(20)30448-4/fulltext
The Environmental Impact of the Healthcare System
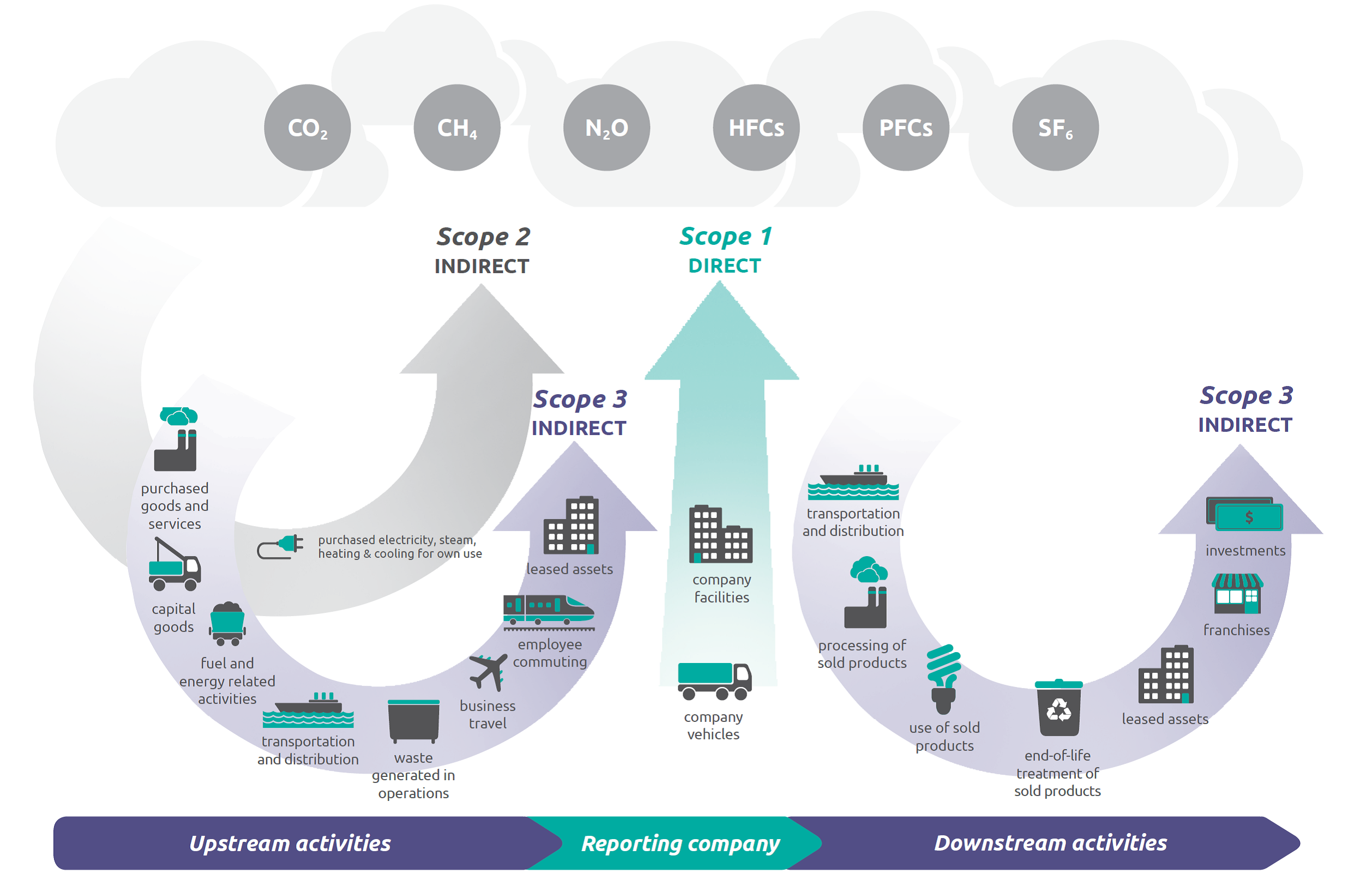
In the United States, the healthcare sector currently accounts for about 8.5% of greenhouse gas emissions, with a significant portion attributed to hospital care and physician services. Health damages caused by pollutants produced by the healthcare sector are commensurate with those caused by preventable medical errors. Sources of greenhouse gas emissions are classified into three scopes:
- Scope 1 emissions are those directly generated by a facility (e.g. from operating room anesthetic gases such as nitrous oxide and desflurane, potent greenhouse gasses)
- Scope 2 emissions are indirect emissions via energy purchased through a utility company, such as electricity.
- Scope 3 emissions, the greatest source of healthcare emissions but also those hardest to track, are those generated by employee activities and the supply chain, such as product transport, waste generation, pharmaceuticals, and employee business travel.
Healthcare produces significant emissions in all three categories. Transitioning towards climate-smart healthcare will require transformational change, including bolstering preventative healthcare and reducing instances of low-value, wasteful care. Organizations such as Health Care without Harm and the National Academy of Medicine Action Collaborative on Decarbonizing the US Health Sector have been working to actualize this transformation, but the health threats posed by climate change require all of us to apply a sustainability lens to every aspect of health care and health systems decision-making.
Quantifying Healthcare Emissions via Life Cycle Assessment
Life Cycle Assessment Methodology
Life Cycle Assessment (LCA) is an internationally-recognized tool to evaluate the environmental impact of a product or process over the course of its lifespan, from raw material extraction to disposal. The four steps of a Life Cycle Analysis are 1) Definition of LCA goal and scope, 2) Inventory analysis, 3) Impact assessment, and 4) Interpretation. These evaluations can identify aspects of clinical practice that have particularly high environmental impact and guide system-level decision-making to reduce waste, emissions, and often, cost. As an example, please see this LCA of hysterectomies led by collaborator Cassandra Thiel.
Stages of a product's life cycle explored by an LCA:
